Lynch syndrome early diagnosis pathway
One aim of the NHS Long Term Plan is that 75% of cancers will be diagnosed at an early stage. This can be achieved through targeted screening and personalised surveillance of those most at risk of developing cancer, such as those with Lynch syndrome.
Each year, 1,100 colorectal cancers are caused by Lynch syndrome, making it the most common form of hereditary colorectal cancer. An estimated 175,000 people have Lynch syndrome in the UK, but fewer than 5% of individuals know they have the condition (Bowel Cancer UK).
For this reason, the National Institute for Health and Care Excellence (NICE DG27 diagnostic pathway) has recommended that all people with colorectal cancer are tested for Lynch syndrome.
Implementing Lynch syndrome pathways nationally provides an opportunity to detect many of these cancers at an earlier stage. It may also help to prevent cancers through risk reduction treatments and appropriate surveillance programmes for patients, and their at-risk family members, who are not yet aware that they have Lynch syndrome and are at risk of developing cancer.
Furthermore, a diagnosis of deficient MMR (dMMR) can affect cancer treatment options, with certain tumours being more responsive to particular chemotherapy agents. People with Lynch syndrome are also responsive to new immunotherapy drugs. It is therefore important that the initial tumour test (IHC or MSI) is done in time to inform treatment options.
To assist healthcare professionals in testing patients for Lynch syndrome, a training programme has been developed to:
- support Trusts across the East of England Region to improve delivery of their local diagnostic pathway for Lynch syndrome
- improve uptake of genetic testing for Lynch syndrome through integration into standard cancer clinics.
This will be achieved by providing training and support to clinicians, so they can identify and consent patients for genetic testing at the routine oncology appointments. Any clinician (i.e. surgeon, oncologist, or nurse specialist) involved in the care of patients with colorectal cancer can complete this training.
The main concern in Lynch syndrome is colorectal (bowel) cancer. Around half of all people with Lynch syndrome develop colorectal cancer. For women, endometrial (womb) cancer is also a concern, and to a lesser degree ovarian cancer. There is small increase in the likelihood of developing a few other cancers: pancreatic, kidney, urinary tract, skin, brain and gastrointestinal cancers. However, these other cancers are seen only occasionally, and the increased risk is small – generally less than a 5% increase if you compare this risk to the rest of the general population.
More information about Lynch syndrome is provided below:
- Lynch syndrome information
- Action needed by cancer services
- Resources for health professionals
- Online training courses
- Useful websites
Lynch Syndrome information
This information has been developed for individuals who have recently been diagnosed with colorectal (bowel) or endometrial (womb) cancer and have been invited for a genetic assessment and possible genetic testing for Lynch syndrome. This is because initial testing of their cancer (tumour) suggests it might have been caused by an inherited condition called Lynch syndrome.
You might have been provided with an information leaflet about your genetics appointment. The information on these pages was developed to provide further detail and may answer most of the questions that you might have about your appointment, or other questions that you might have after your appointment.
It covers the following:
- What is Lynch syndrome?
- How did I get Lynch syndrome?
- Genetic testing for Lynch syndrome
- What does my genetic test result mean?
- Screening and risk reducing strategies
- Will I develop cancer?
- Emotional impact and your family
- Additional support and useful resources for patients
The information on this page is intended to help people who have questions about why they have been referred to genetics, or about the initial tests done on their cancer (tumour). You can also go directly to the sections above that you would like to read more about.
Do I have an inherited condition?
In the majority of cases, colorectal and endometrial cancers are not inherited conditions. In the case of colorectal cancer, it is common in the general population, affecting 1 in 14 men and 1 in 19 women at some point during their life, more commonly after the age of 60.
Most cancers occur sporadically or ‘out of the blue’. However, in about 5-10% (5-10 in 100) of the individuals who develop colorectal or endometrial cancer, cancer is caused by a genetic alteration (a change in their genetic code instructions, or what we are going to call a ‘genetic change’). In about 3% (3 in 100) of all colorectal or endometrial cancers, the genes affected are those whose task is to repair abnormalities when cells are made.
These repair genes (called DNA mismatch repair genes) protect us from developing certain cancer types. This is the case in Lynch syndrome, which is the most common cause of inherited colon and endometrial cancer. It affects 1 in 278 people.
How is Lynch syndrome diagnosed?
It is not straightforward to find out if a cancer is inherited or sporadic (out of the blue). To find out if someone has an inherited cancer that is being passed down in the family, there are different tests that need to be performed. In addition to taking a detailed family history, for Lynch syndrome, some tests are performed on the cancer (tumour) sample. This is because Lynch syndrome leaves a fingerprint in the tumour.
The initial tumour tests are immunochemistry (IHC) and microsatellite instability (MSI):
- Immunochemistry (IHC). Every person diagnosed with colorectal or endometrial cancer has IHC performed on their tumour. IHC looks at the expression of the proteins produced by these ‘mismatch repair’ genes. If there is a loss of expression of any of these proteins, you may be offered genetic testing to find out if you have Lynch syndrome.
- Microsatellite Instability (MSI). This is another type of genetic test on the tumour to find out if you are likely to have Lynch syndrome. If the result is positive, you might have Lynch syndrome, and you will be offered genetic testing.
Additional testing may be required using MLH1 promoter Hypermethylation (MLH1 Methylation). In some cases, following an IHC test, this test might be necessary to clarify if the cancer is sporadic and originates in the tumour cells, or if it could possibly be inherited. If the result of this test shows that the tumour sample is methylated, it clarifies that the cancer is sporadic and originates in the tumour. If not, it is possible that you might have Lynch syndrome and will be offered genetic testing.
If tumour test results show that there is a possibility that you might have Lynch syndrome, you will be offered genetic testing. Genetic testing will be able to confirm if you have Lynch syndrome.
What is Lynch syndrome?
Lynch syndrome is an inherited condition that makes people more likely to develop particular types of cancer. In order to explain Lynch syndrome, we need to explain how normal cells work and divide, and how cancer occurs.
For our body to grow and repair itself, cells must create new cells. If you cut yourself, your skin cells continue to divide until the wound is healed. Normal healthy cells know when to stop dividing. Cancer happens when cells continue dividing when they are supposed to stop. As the cancer cells grow, they begin to crowd out normal cells and eventually form a lump. A lump of cancer cells is called a tumour.
There are some mechanisms in our body that protect us against cancer. These mechanisms guard cells and make sure that the cells know when to stop dividing. When these mechanisms identify cells that are unable to stop multiplying, these mechanisms repair or remove these cells, and by doing so they prevent cancer from occurring. One of these mechanisms is created by the DNA mismatch repair genes called MLH1, MSH2, MSH6 and PMS2.
Everybody has these genes. In Lynch syndrome, one of these genes is not working properly. This means that their cancer protection mechanism is not working at 100%, and so people with Lynch syndrome have less protection against cancer.
These mismatch repair genes work like police officers in our body, checking that cells are made properly and don’t divide and multiply out of control. If these genes aren’t working properly, it might result in fewer police officers, which results in less protection against cancer.
This means that people living with Lynch syndrome have less protection, rather than having a genetic alteration that causes cancer itself. For this reason, not all individuals living with Lynch syndrome will develop cancer, but having less protection makes it more likely. Most people living with Lynch syndrome live a normal life.
Lynch syndrome is caused by a genetic change in one of these DNA mismatch repair genes called MLH1, MSH2, MSH6 and PMS2. There is a fifth gene involved called the EPCAM gene because it turns off the neighbouring MSH2 gene. EPCAM alterations are very rare and only account for 6% of Lynch syndrome cases.
The main concern in Lynch syndrome is colorectal (bowel) cancer. For women, endometrial (womb) cancer is also a concern, and to a lesser degree ovarian cancer. There is small increase in the likelihood of developing a few other cancer types that you may need to keep an eye on, but this will be explained later. The risk or likelihood of developing different cancer types depends on which gene is implicated, and other factors such as gender and age.
Having a diagnosis of Lynch syndrome can be a double-edged sword. On one hand, it could be worrying to know that you have a higher likelihood of developing cancer. On the other hand, you are armed with knowledge and an enhanced screening programme that will help you prevent these cancer types and live a normal and fulfilling life. It will empower you to manage your care. Monitoring and screening will help to prevent cancer, or help to diagnose and treat it early.
It is important to know that you are not alone. As many as 1 in 278 people live with Lynch syndrome. There are over 7 billion people on earth. Over 25 million of them have Lynch syndrome, just like you.
If you would like to meet other people living with Lynch syndrome, there is association called Lynch Syndrome UK run by people living with Lynch syndrome. They have useful resources, organise events, and have online as well as face-to-face support groups where you can meet people just like you.
- Your clinician will tell you about... (see sections 2 to 7)
How did I get Lynch syndrome?
To understand how Lynch syndrome happens, we need to understand DNA and genes. DNA is the code our bodies use to make genes. Genes are the instructions that tell our body how to grow and develop, and each gene has their own job to perform. Some of our genes determine what hair and eye colour we have, and some are responsible for protecting us against diseases like cancer.
Inherited conditions are due to a genetic change (also known as a variant or genetic alteration) in a particular gene, which can be passed on in a family. A genetic change may alter the level of protection a family has against certain diseases such as cancer.
Lynch syndrome is usually caused by a change in the mismatch repair genes. Mismatch repair genes protect us against cancer by repairing DNA mistakes that can occur when our cells are made. The Lynch syndrome genes are like police officers in our body, checking that cells know when to stop dividing and do not turn into cancer cells, and by doing so they protect us against cancer. If these genes aren’t working properly, this might result in fewer police officers protecting us against cancer.
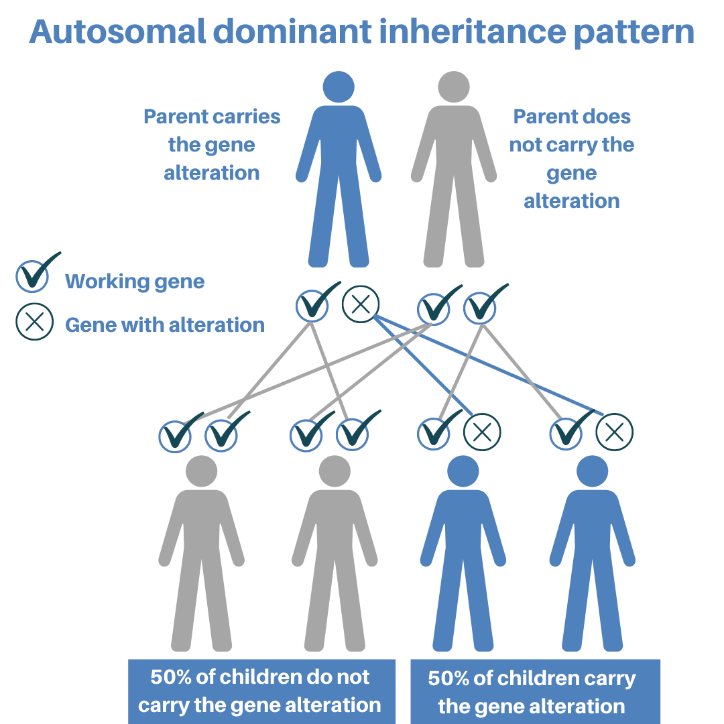
When we are conceived, we inherit two copies of every gene, one copy from our mother and one copy from our father. If one of our parents has Lynch syndrome, at the point of conception, they have a 50% chance of passing on their altered copy and 50% chance of passing on their unaltered copy. If a person inherits the altered copy, they will have Lynch syndrome. This is also known as an autosomal dominant inheritance pattern. This also means a person with Lynch syndrome has a 50% chance of passing on their altered gene each time they have a child.
Figure created by North East Thames Regional Cancer Genetics Service
Mismatch repair genes are inherited from your parents. If you inherit an altered copy of the gene which causes Lynch syndrome, you have Lynch syndrome. Luckily, the copy from the other parent may work just fine. However, there is a chance that one day your working mismatch repair gene will make a mistake in one of the organs affected by Lynch syndrome. When both of your mismatch repair genes are no longer working, you have less protection against cancer, and so cancer will be more likely to occur.
In 99% of cases, you would have inherited Lynch syndrome from one of your parents. In this case, it is possible that your siblings will have it too. If you do not have Lynch syndrome, you cannot pass it on to your children because you cannot pass on something that you don’t have.
It is possible to have Lynch syndrome without inheriting it from your parents, but this is extremely rare. In this case, the genetic alteration happens by nature after conception, and you are the only one that has it. This is called a ‘de novo’ genetic alteration. This would be the first time that Lynch syndrome is found in the family. For this reason, your siblings and parents are unlikely to have Lynch syndrome, but your children will have a 50% chance of inheriting the alteration.
Genetic testing for Lynch syndrome
Genetic testing for Lynch syndrome will involve having a blood test. DNA will be extracted from your blood to look for genetic changes (or variants) that cause disease or increase your risk of developing a disease. This testing takes approximately three months to complete.
Genetic testing for Lynch syndrome helps your doctors to understand you and your family’s risk of developing cancer in the future. Positive test results will also help your doctors to understand the treatments you may require. They will use it to develop an enhanced cancer prevention programme just for you. If you have cancer, you will be eligible for therapies that are known to work best for people with Lynch syndrome, such as immunotherapy.
Having genetic testing is optional. Your decision will not affect the standard of care you receive. However, knowing you have Lynch syndrome will give you and your family access to personalised cancer prevention programmes, advice and treatments. It will also enable testing of other family members and, if appropriate, they will also be provided with a personalised cancer prevention programme to help reduce the chance of further cancers developing in the family.
Genetic results
Genetic test results do not always give a clear answer. This is because the science of genetics is still in its infancy. For this reason, and for clarity, your results will be classified as positive, uncertain or negative:
- Positive: a genetic change for Lynch syndrome is identified
This result would confirm the diagnosis of Lynch syndrome and provide an explanation for why you developed cancer. Your cancer team will use this information in their management decisions and will discuss this with you further. You might be considered for additional therapies, and they will offer predictive genetic testing to your first-degree relatives (parents, siblings and children), as they might carry the same genetic change. - Uncertain: Genetic change (or variant) of unknown clinical significance is found
A genetic change is found, however it is not certain that it is the cause of your cancer. If appropriate, there may be further analysis of your tumour or other family studies recommended. Unfortunately, genetic testing cannot be offered to your family members at this time but cancer surveillance for you and your family will still be recommended. - Negative: No genetic changes were found
This result doesn’t rule out an inherited condition. It might be that the limited knowledge we have about genetics means we are unable find a genetic change currently. If appropriate, there may be further analysis of your tumour recommended, to try to clarify if you have Lynch syndrome. Unfortunately, genetic testing cannot be offered to your family members but cancer surveillance for you and your family will still be recommended. Screening recommendations for you and your family will follow the Lynch-like syndrome recommendations, which your clinician will tell you about.
What does my genetic test result mean?
After approximately three months you will be given your genetic test results. You have been waiting for this and these three months might feel like a long time. Now that you have spoken to your team and have your results, you might have some questions.
Please read the information below as many times as you need so you can understand your results and its implications for you and your family and, most importantly, what can you do to reduce your prevent cancer and balance out the risk.
The main concern in Lynch syndrome is colorectal (bowel) cancer. For women, endometrial (womb) cancer is also a concern, and to a lesser degree ovarian cancer. There is small increase in the likelihood of developing a few other cancers: pancreatic, kidney, urinary tract, skin, brain and gastrointestinal cancers. However, these other cancers are seen only occasionally, and the increased risk is small – generally less than a 5% increase if you compare this risk to rest of the general population.
The risk or likelihood of developing cancer depends on three factors: age, gender and which gene is implicated:
- Age
The likelihood of developing cancer is very low at an early age, including for people with Lynch syndrome. Cancer prevention bowel check-ups for people living with Lynch syndrome start at the age of 25-35. The likelihood of developing cancer increases with age, so people with Lynch syndrome will have bowel checks every two years. - Gender
Men tend to have a higher risk of developing colorectal cancer as compared to women. However, women have the additional risk of endometrial and ovarian cancer. - Gene
Different genes have a different likelihood of contributing to the development of cancer. There are some websites that can give you percentages of risk. It can be difficult to look at graphs and make sense of the information, especially when the information is personal to you. If you do wish to calculate your risk, it is recommended to do this with a healthcare professional, who can interpret and personalise the information for you and answer your questions appropriately. However, if this is something that you would like to look at on your own, you can visit the Prospective Lynch Syndrome Database.
Screening and risk-reducing strategies
Below are some of the general screening recommendations and cancer prevention strategies for Lynch syndrome. Your healthcare professional will explain and go through your personalised cancer prevention programme with you in more detail. Your personalised cancer prevention programme will include your gene specific recommendations which are not included here. If you have any questions, get in touch with your healthcare team.
- Consider taking aspirin (NICE guidelines 2020) from the age of 25 to 65 for cancer prevention: Aspirin has been shown to reduce the long term risk of cancer in Lynch syndrome by around 50%. Trials to determine the best dose of aspirin for cancer prevention are still ongoing, so discuss with your GP whether you have any contraindications to taking aspirin before you start. If you are younger than 25 and you wish to start taking aspirin, discuss this with your medical team. [Lynch syndrome: should I take aspirin to reduce my risk of getting bowel cancer. Patient decision aid, NICE, 2020]
- One-off screening for Helicobacter pylori: H. pylori is a bacteria that 30% of the population have in the stomach. Eradication of these bacteria may reduce the lifetime risk of gastric cancer by half. To arrange testing for this contact your GP.
- General lifestyle recommendations:
- Healthy diet: High fibre, low fat, with plenty of fruit and vegetables. Try to eat less red and processed meat. It is also good for your general health that you include starchy foods in your diet such as plantains and green bananas.
- Behaviours: Limiting your alcohol intake, not smoking, and doing regular exercise is beneficial for your general health and all have a role in preventing the development of cancer.
- Body weight: Maintaining a healthy body weight is also important.
- Two-yearly check-up of your bowel: For colorectal cancer prevention.
- Gynaecological surveillance: Currently there is limited evidence to support gynaecological surveillance for the early detection of gynaecological cancer in Lynch syndrome. There are some surgical risk-reducing interventions available for women between the ages of 40 and 45 who have completed their family. Please discuss this with your healthcare professional.
- To prevent or reduce the risk of developing other cancer types, such as skin cancer, we recommend symptom awareness and to remain vigilant. If you have a new symptom that lasts for over 2 weeks, it is recommended that you seek medical advice.
Will I develop cancer?
To explain what the likelihood is that someone living with Lynch syndrome will develop cancer, we first need to explain what the likelihood is that someone in the general population will develop cancer.
What does it mean when my doctor or nurse talks about cancer in the general population?
Unfortunately, cancer is common, and in the majority of cases is not inherited. As many as 1 in 2 people will develop cancer in their lifetime. That is 50% of the world’s population.
Most cancers are not inherited and occur out sporadically or ‘out of the blue’. Their origin is based on the tumour cells themselves. Some common reasons for cancer are ageing, exposure to chemicals, radiation, hormones or other factors in the body or environment. Sporadic cancers usually occur at a later age in life because people are not born with a predisposition, and the development of cancer usually takes many years to generate.
It’s important to be aware of this because nobody is free from cancer risk. When clinicians explain to people with inherited cancer predisposition syndromes that they have an increased likelihood of developing certain cancer types, they make comparisons to the general population, so it is helpful to know that everyone is at risk to some extent.
If you are reading this, and you don’t have an inherited cancer predisposition syndrome, it is important to still take steps to prevent cancer from occurring. For instance, take part in national cancer prevention programme such as the National Bowel Cancer Screening programme or the National Cervical Cancer Screening Programme if you are eligible and invited to participate.
Likelihood of developing cancer in Lynch syndrome
The risk or likelihood of developing cancer is there, even in the general population. Lynch syndrome makes certain (not all) cancer types more likely to develop. This is due having less protection from the cancer mismatch repair genes. This doesn’t mean that you will definitely develop cancer, but having less protection makes it more likely.
However, there is a way in which you can balance out this increased likelihood, and that is by taking control and remain vigilant. If you have a new concerning symptom (such as a change in bowel habit, unusual bleeding in between menstrual periods, lumps/swelling in the abdomen, or new/changing or unusual skin growth or lesion) that last for over 2 weeks, we recommend that you seek medical advice.
In addition, it is recommended that you take control of your personalised surveillance programme, and follow a healthy lifestyle that will help you to reduce, and balance out, this increased risk of developing cancer, or at least enable it to be detected and treated early. If you have been diagnosed with Lynch syndrome, you can find some general recommendations in the Screening and risk reducing strategies section. Your team will discuss these recommendations, and some other gene specific recommendations, with you.
Not everyone living with Lynch syndrome will develop cancer. The chance of developing cancer is considerably lower in individuals who know that they have Lynch syndrome and follow their enhanced screening programme, compared to individuals who have Lynch syndrome but are unaware of their diagnosis. This is because knowing about the risk gives individuals the chance to take action in a timely manner, and can help to ensure that cancer is detected at an early stage so it can be treated more effectively.
It is important to highlight that Lynch syndrome doesn’t usually affect children. This is why the enhanced cancer prevention programs for Lynch syndrome starts between the ages of 25 to 35. The start age of your family cancer prevention programme will depend on which gene is implicated. For instance, individuals with genetic changes in the PMS2 gene have a lower likelihood of developing cancer compared to those who have a genetic change in the MLH1 gene.
However, what really makes a difference is to follow your personalised screening programme, and make sure you make the most of your regular check-ups. In any case, if you have a family history of earlier onset of cancers, make your clinician aware, as you and your family might begin screening a little earlier.
In addition to that, regardless of the age in which your cancer prevention programme starts, it is important to always be symptom aware and to remain vigilant. If you have a new symptom that lasts for over 2 weeks, it is recommended that you seek medical advice, regardless of your age.
It is impossible to know your exact risk or likelihood of developing cancer due to Lynch syndrome because other factors influence the risks such as lifestyle, the foods you eat, and environmental toxins. The way Lynch syndrome behaves in you and your family can be very different as the affected Lynch syndrome genes interact with other genes as well. Family history should be taken into consideration, but each family member will be affected differently.
There are other general lifestyle recommendations that will reduce your likelihood of developing cancer. You can find these lifestyle recommendations in the gene-specific information in the Screening and risk reducing strategies section.
Is there a cure?
There is no cure for Lynch syndrome, but your clinicians will help you put together a personalised screening programme that will help you manage Lynch syndrome so you can balance out your increased risk of cancer and live a normal life.
I have Lynch syndrome and I have already had cancer. Can I get cancer again?
Yes, cancer can happen again. This is why is important to follow your personalised cancer prevention programme, as this will significantly reduce your risk of cancer, or catch it and treat it early.
Emotional impact and your family
Finding out that you have Lynch syndrome can be challenging. It could be an additional worry as this diagnosis not only affects you but also the rest of your immediate family. To know that you have Lynch syndrome is also life-saving information for you and your family, as it will empower you and arm you with a personalised enhanced cancer screening programme that could prevent future cancers, or at least help detect them and enable them to be treated early so you can have a normal and fulfilling life.
It is very important that you tell your parents and siblings about your diagnosis, as they have a 50% chance of having the same genetic change. They need to know as they could have Lynch syndrome too, and this information can help them to take steps to prevent or reduce their risk of developing cancer. Your healthcare professional can help you think about how to have this conversation and share this information, and give you a letter to pass on to your family so they can have the genetic blood test to find out if they have Lynch syndrome or not. If they have Lynch syndrome, their extended family will also be risk.
Perhaps one of the most difficult decisions is how to tell your children and how to approach the conversation as they also have a 50% chance of having Lynch syndrome. Deciding how and when to have this conversation can be difficult.
Genetic testing is not recommended for children younger than 18. It is recommended that you answer your children’s questions using language that is easy for them to understand, and share the information when you feel they are ready to learn about Lynch syndrome. Younger children might not understand what your diagnosis means to them. Children differ in the age in which they are ready to learn about Lynch syndrome and their risk of developing cancer.
In most cases, children cope better when the family is willing to discuss what is happening. This helps them feel valued and respected. Remember that not everyone living with Lynch syndrome will develop cancer, so your children might not develop cancer. Also, cancer treatments, screening and risk reducing strategies improve over time, so the options that will be available to your children when they become adults might be even better than now. Furthermore, if your children have Lynch syndrome and they wish to have children, they will have additional family planning options open to them if they wish to not pass on Lynch syndrome.
Many people are preoccupied when sharing this information because they are concerned how their relative is going to react. People are concerned about causing anxiety to their family and can feel anxious, guilty or responsible about causing this upset. It is always difficult to share what is considered to be bad news. It can help to think about other times when you share bad news, or think about the benefits of having this information, such as helping your relatives to find out if they have Lynch syndrome, and if they do, to help them to take steps to prevent cancer, as this is life-saving information.
It is important to remember that you are not responsible for having Lynch syndrome. This happens by nature and it has been passed on to you from your parents, and your parents from their parents and so on. Also, we cannot control the genes that are passed on to our children, and you didn’t know that you have the Lynch syndrome when you decided to have children. You cannot take responsibility for something that you didn’t know about.
Sometimes sharing this information can be burden. You can ask other close family members to help you talk to the rest of the family, or to give your family the letters and other information that they need to get tested. Also, remember that your healthcare professionals might be able to help develop strategies to share the information.
Additional support and useful resources
Living with Lynch syndrome can be a double-edged sword. On one hand, it could be worrying to know that you have a higher likelihood of developing cancer. On the other hand, you are armed with knowledge and with an enhanced screening programme that will help you prevent these cancer types and live a normal and fulfilling life. It will empower you to manage your care and reduce the risk of cancer, or enable it to be detected and treated early.
It is important to know that you are not alone. There are many people in the UK who live with the same syndrome, just like you, and live a fulfilling life.
If you would like to meet other people living with Lynch syndrome, there are associations that can help you get in touch with people just like you. They have useful resources, organise events, and online as well as face-to-face support groups such as Lynch syndrome UK.
Additional sources of emotional support
There are additional sources of emotional support. If you would like additional support, we suggest that you discuss your wishes with a member of your healthcare team who will be able to help you, or choose and signpost you to the right service.
Below are some of the services available with information about what they offer and how to contact or self-refer to them.
One-to-one therapy: If you would like to access one-to-one therapy, there is a national programme called Improving Access to Psychological Therapy (IAPT). You can self-refer to this service.
- Click on the link and enter your postcode and click ‘start now’.
- It will give you some information about what happens when you self-refer – Click ‘Continue’.
- Enter your GP postcode and you will get a list of service providers.
- Select a service that you can self-refer to and follow the instructions (either fill in the online form or call).
- Someone from the psychological therapies service will get in touch and will give you more information.
Macmillan Support Line: The Macmillan Support Line offers confidential support to people living with cancer and their loved ones. The telephone line is open 8am to 8pm: 0808 808 00 00. There is also an email and online chat function.
Breathing space: Free, confidential, web-based service for people experiencing low mood, depression and anxiety. Tel: 0800 83 85 87
Samaritans: Free, confidential, web-based service providing emotional support to anyone in emotional distress, struggling to cope, or at risk of suicide. Tel: 116 123
Togetherall: Free in some London areas. For anxiety and depression and other common mental health issues. Also provides social support groups.
Apps for relaxation, stress reduction and anxiety management
- Calm
- Headspace
- Feeling Good app
- PZIZZ provides help with sleep hygiene
- CATCH IT provides help with negative thoughts
- WorryTree to help manage your worries
- Motivation apps to remain active, drink less, easy meals, smoke cessation, etc
Insurance
If you have been diagnosed with cancer, and you are having genetic testing, you are having a diagnostic genetic blood test. This might confirm your diagnosis of Lynch syndrome.
If you apply for a new insurance after your diagnostic genetic test, companies can ask you about your medical history and any diagnosis that you have. They will also ask you about your family history. You will have to disclose any health condition that has been diagnosed by genetic testing. However, what is likely to affect your insurance assessment is your cancer diagnosis and family history, even if you recovered from the cancer and treatment has been completed.
What is important to know is that you do not need to disclose that you have a genetic test or your results to any insurance company for the policies that you already have in place.
If you have any questions about how your genetic test could affect your insurance, more information is available from:
- The Association of British Insurers
- The Code on Genetic Testing and Insurance
- Insurance implications for family members that do not have cancer and are going to have a predictive genetic blood test are different. More information is available from Genetic Alliance UK.
What do cancer services need to do?
1.All trusts should appoint an individual to take on responsibility for implementing this pathway. The Cancer Alliance has written out to all Colorectal & Endometrial Cancer MDTs asking them to nominate a ‘Lynch Lead.’ This lead is well placed to also champion implementation of the Lynch pathway across various specialties and the Alliance has also asked for other specialities, where we know Lynch may be implicated, to be part of pilot lynch test pathways.
2.Establish a regional Lynch network to support and develop the delivery of a cross-system service. Bring together key stakeholders (pathology, endoscopy, GLHs, clinical genetics service, cancer team, surgical team, Genomic Medicine Service Alliances and Cancer Alliances) bi-annually as part of a Lynch syndrome network to review delivery of service standards and to support service development.
3.Develop regional expert centres who will be able to provide clinical advice and training to dedicated local leads within cancer MDTs and manage regional patient registries.
4.Identify how you will ensure patient and carer feedback is welcomed, listened to and acted upon throughout the pathway as a measure of experience of care
5.Work with GPs to prepare for a rise in the number of people presenting and asking for a referral to the genetics service due to risk of Lynch syndrome. Make sure they are aware of referral pathways and who to signpost any questions on to.
Information for patients
Patient information leaflet
Consent record of discussion
Testing
SOP
Impact Report
Implementing testing and surveillance pathways
Virtual Hereditary Colorectal Cancer MDT proforma
Example results letter
This document has been created to give an idea of what to write in the genetic results letter. It is not intended to use as a template, but rather to give an idea on how a genetic result letter could be written
Lynch syndrome guidelines
- Guidelines for the management of hereditary colorectal cancer
- The Manchester recommendations for the management of gynaecological cancers in Lynch syndrome
- NHS England Implementing Lynch syndrome testing and surveillance pathways July 2021
- Lynch Syndrome Guidance for Primary Care Clinicians
Lynch syndrome patient resources
- Patient leaflet: Information for Patients with Colorectal Cancer (updated July 2021). This document is mentioned in the training. Ideally, it should be given to eligible patients prior their appointment for genetic counselling for Lynch syndrome.
- Patient specific web page: If your patient has further questions about Lynch syndrome or genetic testing you can direct them to the dedicated patient specific information web page, https://rmpartners.nhs.uk/lynch-syndrome-information/ (the link for this website can also be found in the patient leaflet above).
To assist healthcare professionals in testing patients for Lynch syndrome, the National Lynch Syndrome Project Team have developed a training programme to:
- support Trusts across East of England to improve delivery of their local diagnostic pathway for Lynch syndrome
- improve uptake of genetic testing for Lynch syndrome through integration into standard cancer clinics.
This will be achieved by providing training and support to clinicians, so they can identify and consent patients for genetic testing at the routine oncology appointments. Training is available as follows:
- Training for MDTs Option 1: Suitable for MDT members to help them identify patients likely to have Lynch syndrome and refer these patients to genetic testing.
- Training for MDTs Option 2: Suitable for MDT members to help them identify patients likely to have Lynch syndrome, offer genetic testing to these patients, and manage their care after receiving the genetic test results.
- Training for Pathologists
- Training for Primary Care Clinicians
- Supporting documents
Clinician Lynch syndrome online training
The clinician training involves watching six short videos which cover all the different stages of the Lynch syndrome pathway, and then completing an online questionnaire to ensure that the clinician has understood correctly the processes and procedures for testing have been understood correctly. In addition, there is a range of supporting documents to help understand this pathway.
Lynch syndrome (colorectal cancer) online training for MDTs: Option 1
The training below covers the modules required for members of the MDT that have chosen to follow option 1 of the pathway.
Option 1 of the pathway will help you to:
- identify patients likely to have Lynch syndrome
- refer these patients for genetic testing to either:
Each MDT should choose to offer either genetic testing via:
- referring patients to their linked specialised genetics centre
- your mainstreaming service ‘in-house’ (if you have set up one)
The training involves watching four short videos which cover all the different stages of the Lynch syndrome pathway, and then completing an online questionnaire to ensure that the clinician has understood correctly the processes and procedures for testing. In addition, there is a range of supporting documents to help understand this pathway.
The training videos cover:
Module 1: Introduction (Introduction to mainstreaming cancer genetics)
Module 2: Lynch syndrome (Genetic testing for Lynch Syndrome)
Module 3: Tumour testing & identifying patients eligible for genetic testing
Module 4: Taking a genetic family history & drawing a family pedigree
Module tests
- Click here to take the test for Module 1
- Click here to take the test for Module 2
- Click here to take the test for Module 3
- Click here to take the test for Module 4
Once you have completed the questionnaires, please email Laura Monje-Garcia, Nurse Practitioner, The St Mark’s Centre for Familial Intestinal Cancer, at LNWH-tr.SMCFIC@nhs.net if you have any questions or comments. She will review your answers and send you the CPD training certificate if you have passed.
Lynch syndrome (colorectal cancer) online training for MDTs: Option 2
The training below covers the modules required for members of the MDT that have chosen to follow option 2 of the pathway.
Option 2 of the pathway will help you to:
- identify patients likely to have Lynch syndrome
- offer genetic testing to your patients
- manage your patients care after the genetic results
The training involves watching six short videos which cover all the different stages of the Lynch syndrome pathway, and then completing an online questionnaire to ensure that the clinician has understood correctly the processes and procedures for testing. In addition, there is a range of supporting documents to help understand this pathway.
The training videos cover:
Module 1: Introduction (Introduction to mainstreaming cancer genetics)
Module 2: Lynch syndrome (Genetic testing for Lynch Syndrome)
Module 3: Tumour testing & identifying patients eligible for genetic testing
Module 4: Taking a genetic family history & drawing a family pedigree
Module 5: Genetic counselling & sending the blood sample for genetic testing
Module 6: Managing genetic results
Module tests
- Click here to take the test for Module 1
- Click here to take the test for Module 2
- Click here to take the test for Module 3
- Click here to take the test for Module 4
- Click here to take the test for Module 5
- Click here to take the test for Module 6
Once you have completed the questionnaires, please email Laura Monje-Garcia, Nurse Practitioner, The St Mark’s Centre for Familial Intestinal Cancer, at LNWH-tr.SMCFIC@nhs.net. She will review your answers and send you the CPD training certificate if you have passed.
Lynch syndrome online training for pathologists
This Lynch syndrome online training for pathologists was created by Dr Nicholas West, Associate Professor of Pathology and Honorary Consultant in Gastrointestinal Pathology, University of Leeds. It covers the modules required for pathologists.
Please note that the training videos cover both the colorectal cancer and endometrial cancer pathways. For this reason, it is recommended that you take your cancer pathway specific modules and tests only.
The training involves watching two short videos which cover all the different stages of the Lynch syndrome pathway, and then completing the two related online questionnaires to ensure that you have understood correctly the processes and procedures for testing. In addition, at the end of the page you will find a range of supporting documents to help understand this pathway.
Colorectal cancer: Modules 1 & 3
- Video 1: Online training for pathologists: testing pathways in colorectal cancer
- Video 3: Online training for pathologists: interpretation of mismatch repair immunochemistry
Endometrial cancer: Modules 2 & 3
- Video 2: Online training for pathologists: testing pathways in endometrial cancer
- Video 3: Online training for pathologists: interpretation of mismatch repair immunochemistry
Module tests
- Click here to take the test for Module 1
- Click here to take the test for Module 2
- Click here to take the test for Module 3
Once you have completed the questionnaires, please email Laura Monje-Garcia, Nurse Practitioner, The St Mark’s Centre for Familial Intestinal Cancer, at LNWH-tr.SMCFIC@nhs.net if you have any questions or comments. She will review your answers and send you the CPD training certificate if you have passed.
If you would like to find out more about Lynch syndrome or the genetic counselling process, we recommend you continue with the online training for the colorectal or endometrial MDTs Option 1.
Pathology specific supporting documents
Lynch syndrome online training for primary care clinicians
The training below will help you manage your Lynch syndrome patients as they first present to you.
The training involves watching a short video which covers:
- A brief overview of Lynch syndrome
- Their personalised cancer prevention programme
- An introduction to the Lynch syndrome quick guide and how it can help you identify and manage your patient’s care
- How to manage their first-degree family members’ care
Video 1: Lynch syndrome quick guide module for primary care clinicians
After you complete the module click here to take the test for module 1.
There is a ‘Lynch syndrome quick guide for primary care clinicians’ document available below. We suggest you download a copy to review while you are watching the video.
Risk Calculator
Prospective Lynch Syndrome Database - calculation of cumulative risk for cancer
Insurance information for patients:
ABI - about the Code on Genetic Testing and Insurance
Access the Code on Genetic Testing and Insurance
Insurance implications for family members that do not have cancer and are going to have a predictive genetic blood test are different. More information is available from Genetic Alliance UK.
Support:
Lynch Syndrome UK - a charity to help sufferers of Lynch Syndrome